Written by: Lindsay Peltsch RN, BScN
Contributions from: Dr. Harley Eisman MDCM, FRCPC
Drowning. The word itself is charged and creates a visceral emotion for most parents. As pediatric nurses and doctors (who are also parents), we have seen this tragedy firsthand. We understand the very real fear of your child drowning, and don’t want it to become a reality for anyone. Our responsibility in frontline healthcare is to not only treat illnesses and concerns as they arise, but to PREVENT things before they happen though education. In pediatrics, we have a powerful ally that no other area of medicine has…you!. Parents and caregivers are an advocate group like no other, eager to work as a team to prevent harm to their children. For us, it is tremendously rewarding to empower this team through education. Sometimes though, a healthcare provider’s well-intended explanation of an issue can take on a life of its own and accidentally cause panic among caregivers instead of empowerment. Examples of this are the terms “dry drowning,”, or “secondary drowning.”
An article about “secondary drowning” or “dry drowning” started making its rounds in 2017. It detailed the terrible stories of children that had a fairly normal day at the pool or beach, spluttered after going under once, but returned home seemingly well. In the hours following, they became progressively sicker, and died. Losing your child is every parent’s biggest fear, but the added terror of potentially missing the warning signs when you think they are ok? New parenting fear unlocked. For most parents, it is easy to think back to the times your own child has choked on a mouthful of water, recovered, and ultimately carried on with their day. When you can personalize a tragedy, the fear grows deep roots in our psyche as parents. It’s difficult to overcome once it takes hold.
“The term secondary drowning or dry drowning should not be used, as it is a misnomer, and causes undue anxiety for parents and many unnecessary visits to the Pediatric Emergency Department” – Dr. Harley Eisman
It has been widely documented by pediatricians everywhere that these two terms are not medical terms. The tragic scenarios depicted in the media are actually called an aspiration event. Certainly not anything to take lightly, but the term itself is enough to deflate the anxiety surrounding it. So we can learn what it is – and how to spot it. KixCare’s chief medical officer Dr. Harley Eisman, has worked as a pediatric emergency physician for over 25 years at Montreal Children’s Hospital. He remembers when these articles started to circulate and the term began to be adopted routinely. He and many of our pediatric colleagues share frustration with how this term created an increase of misinformation among worried parents.
What Is Drowning?
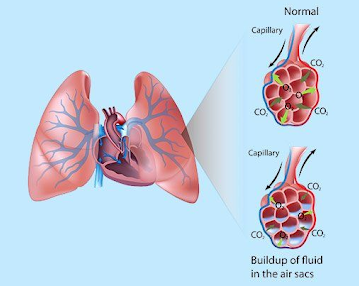
Drowning is when a child breathes in water, and that water fills up the tiny sacs in the lungs (alveoli). When there is fluid in the sacs, normal exchange of oxygen and carbon dioxide can’t take place. Drowning doesn’t always mean death. The amount of fluid that fills the lungs will determine whether the child can exchange any oxygen. The more fluid they take in, the more likely there is to be a fatal outcome. This happens within seconds and minutes. It is why you must always watch children around water.
KixTip! – If you lose track of your child during the day, even if you aren’t at the pool, the FIRST place you should check is any available water source (pool, lake, pond, bathtub). Literally every second counts. The majority of children who drown are fully clothed, meaning they weren’t “swimming” when the event occurred. There are many other less obvious drowning risks that are part of our daily life. Head over to our Instagram to read more.
If your child has a prolonged submersion event, requires resuscitation, loses consciousness, and/or has blue lips at any point, you must call 911 or go to the emergency room immediately. This is a drowning event.
What Is An Aspiration Event?
Aspiration is a broad term for when any liquid or solid enters into the lungs. This can be anything from a drink like water, to food such as a popcorn kernel (more on that another day). However, there is always a risk of complications from aspiration, regardless of what substance is inhaled. In this case, we are talking about the aspiration of swimming water. The key to remember is that aspiration is our body’s reaction to a foreign substance in our lungs. Whereas drowning happens when water blocks the lungs’ ability to work.
How Does it Happen?
Our human bodies are amazing things. Since our lungs only like to have air in them, our body has many systems in place to keep everything else out. We have a flap (called the epiglottis) that automatically covers the entrance to our lungs when we swallow – think of it as a trap door.
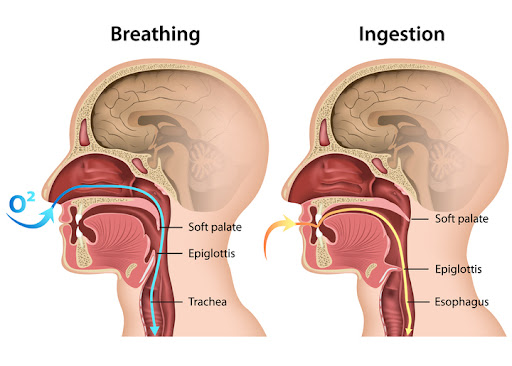
IF something threatens to get past that trap door, our body has another defense – coughing! Have you ever had a sip of water “go down the wrong tube?”. Your body will cough forcefully – even until you vomit if necessary – to clear the perceived threat to the lungs. This may feel terrible, but shortly it passes. THAT is your amazing body doing its job, preventing aspiration!
However, when something sneaks past the epiglottis and gets into the lungs, it sits there over time and the lung tissue itself can become inflamed/irritated (swollen) or an infection can start. This doesn’t always happen right away, it progresses over time. This can cause respiratory distress, and can progress to serious complications left untreated. This is not as common as the news portrays, but there are always early symptoms to look out for in order to be safe.
How Do I Know What to Look For?
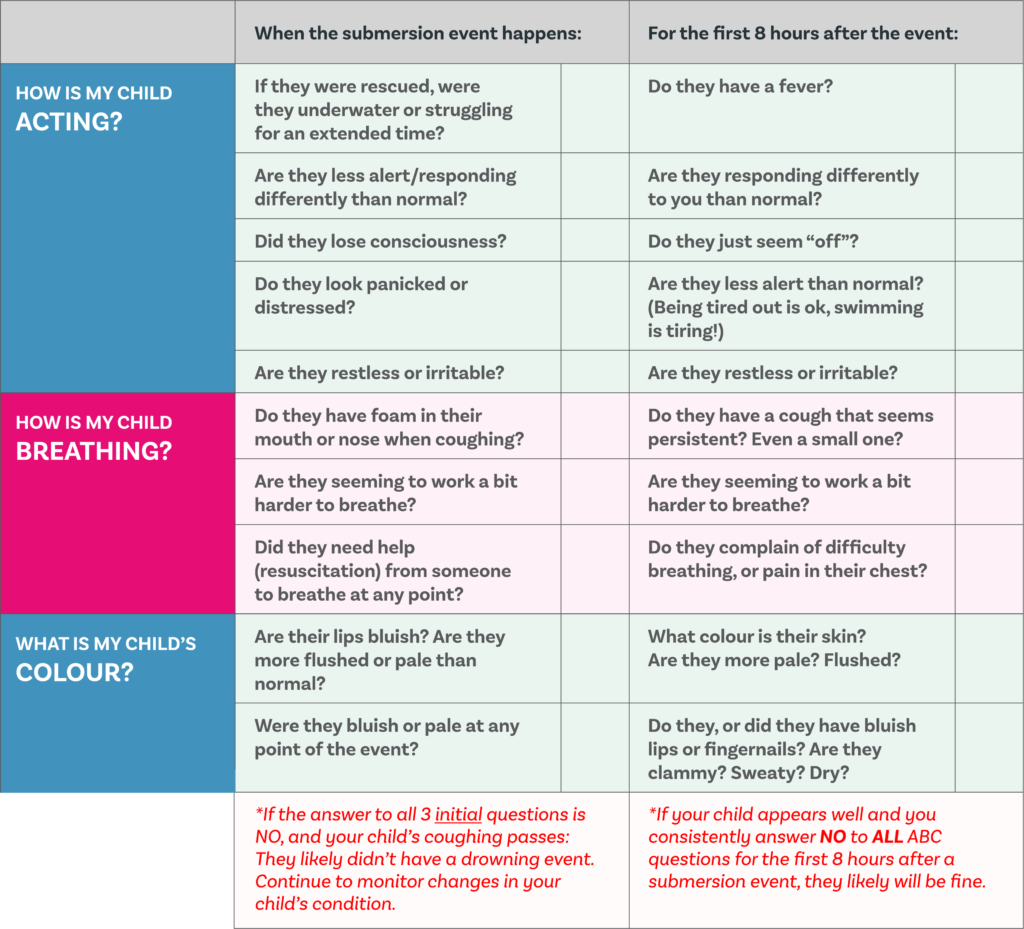
Luckily, these symptoms are easy to spot if you know what to look for, and are easily treated when caught early. Pediatric assessment is like putting together pieces of a puzzle. No single piece can show you the whole picture. As you put them together, you begin to get an idea of what it might be. While it can take up to 24-48 hours for a full aspiration picture to emerge, small puzzle piece symptoms reveal themselves sooner. These are the same principles that experienced pediatricians, paramedics, nurses, and emergency doctors use every day to quickly get an idea of how a child is doing. The trick to good pediatric assessment is that you keep doing it. The more you practice, the more you will do it instinctively and notice small signs.
We created 3 easy-to-remember questions to identify those tricky puzzle pieces: the ABC’s of aspiration assessment
How is my child Acting? How is my child Breathing? What is my child’s Colour?
- If your child appears well and you consistently answer NO to ALL ABC questions for the first 8 hours after a submersion event, they likely will be fine. However, if something seems off, please go to the emergency department.
- If you answer YES to ANY of these questions at any point, even if they were fine before or if you were unaware it occurred: You should proceed to the emergency room to have your child be checked out.
Aspiration events related to swimming are extremely rare. Using these three simple questions, you can be empowered to enjoy the water and trust your child’s body to tell you when something is wrong. By debunking the myth of dry drowning, we can promote effective water safety. Let’s prioritize education, prevention, and responsible supervision to create a safe environment where children can enjoy the benefits of water activities without unwarranted anxiety.
If you are not sure about your assessment, our Kix360 subscription allows you to text an experienced pediatric nurse 24/7 on demand. They can talk through the scenario with you, do a video assessment, help create a plan, and will follow up regularly until your child is recovered. After all, peace of mind is priceless..



![Verify Approval for [YOUR-WEBSITE-URL].com](https://static.legitscript.com/seals/11167439.png)
